In the aftermath of the devastating flooding at Camp Mystic, many families in our community are facing overwhelming emotions, from grief and fear to uncertainty and anxiety. Children and teens, in particular, may be struggling to process what has happened.
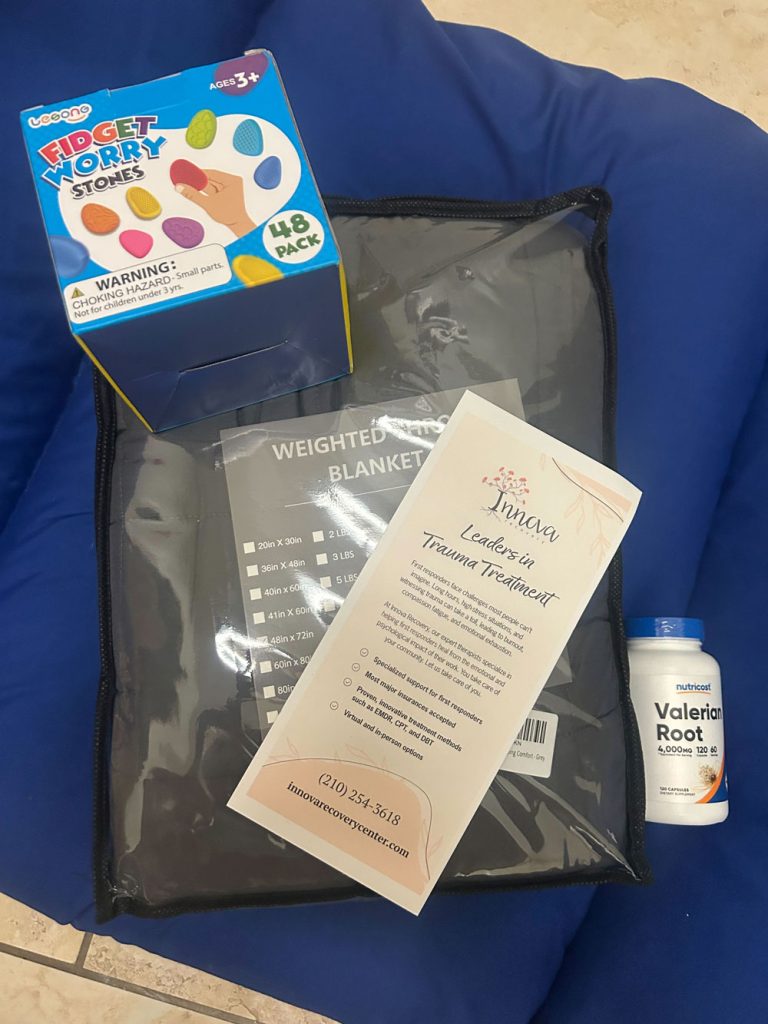
At Innova Recovery Center, we know that early support is key to helping young people navigate trauma in healthy, effective ways. As leaders in trauma treatment and as Texans committed to serving our neighbors, we are honored to offer free virtual group therapy sessions for Camp Mystic flood victims and their siblings, from kindergarten through 12th grade.
What These Groups Offer
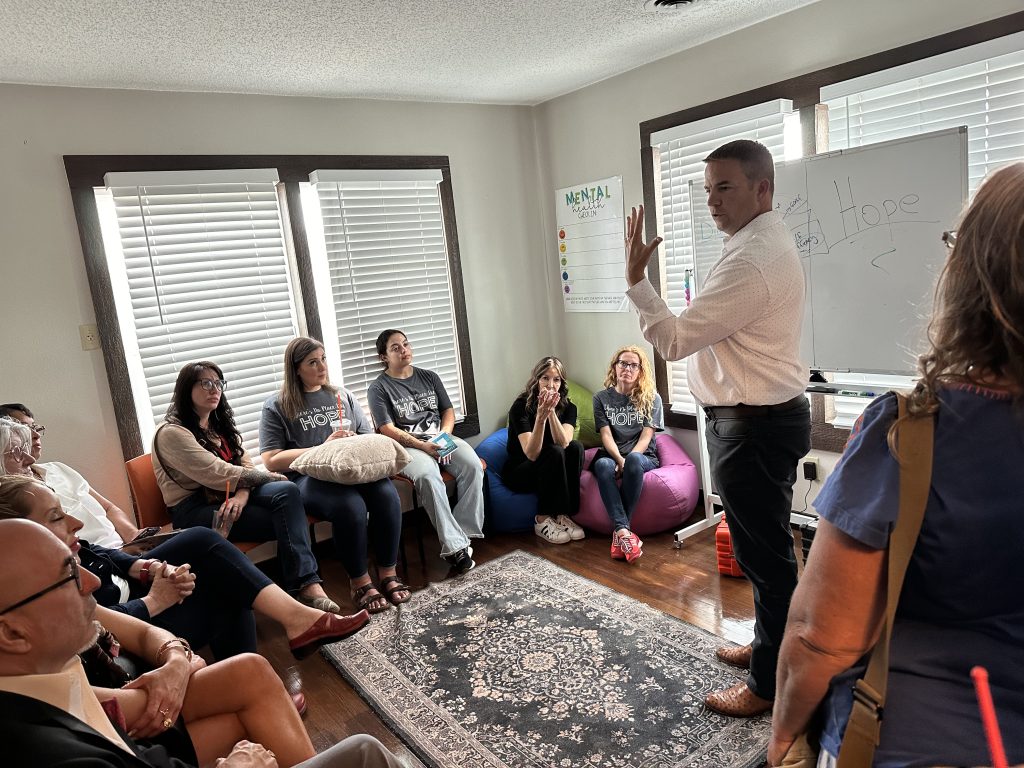
Led by trauma-trained therapists, these virtual sessions provide a safe, nurturing space for kids and teens to:
- Begin processing their experiences
- Learn healthy coping skills to manage anxiety, fear, and grief
- Connect with peers who understand what they’re going through
- Build resilience through Crisis Intervention & Stress Management (CISM) tools
Whether your child is feeling anxious, withdrawn, or simply needs a safe place to talk, these groups are designed to meet them right where they are, with compassion and clinical care.
Group Details
Sessions are held virtually via secure telehealth every week at the following times, organized by age group to ensure appropriate support:
- K through 5th Grade:
- Tuesday and Thursday
- 10:00 AM
- Starting July 15
- 6th through 12th Grade:
- Wednesday and Friday
- 12:00 PM
- Starting July 16
Each session will be facilitated by licensed, trauma-focused therapists who are dedicated to helping children and teens start their healing journey in a safe and supportive environment.
How to Register
If your child or teen would benefit from participating in these free therapy groups, we encourage you to reach out to us immediately:
Call or Text: (210) 254-3618
Email: admin@innovarecoverycenter.com
We’re Here for You
These sessions are offered completely free of charge as part of Innova’s commitment to stand alongside our community during this difficult time. We believe that no family should face trauma alone, and this is our way of helping those impacted take the first step toward healing.
At Innova, we understand that healing takes time, and it’s a journey best undertaken together. Whether you need help for your child, yourself, or your family, please know we are here to walk alongside you every step of the way. Please don’t hesitate to contact us. You can also learn more about our relief efforts and resources here.
Together, we heal.